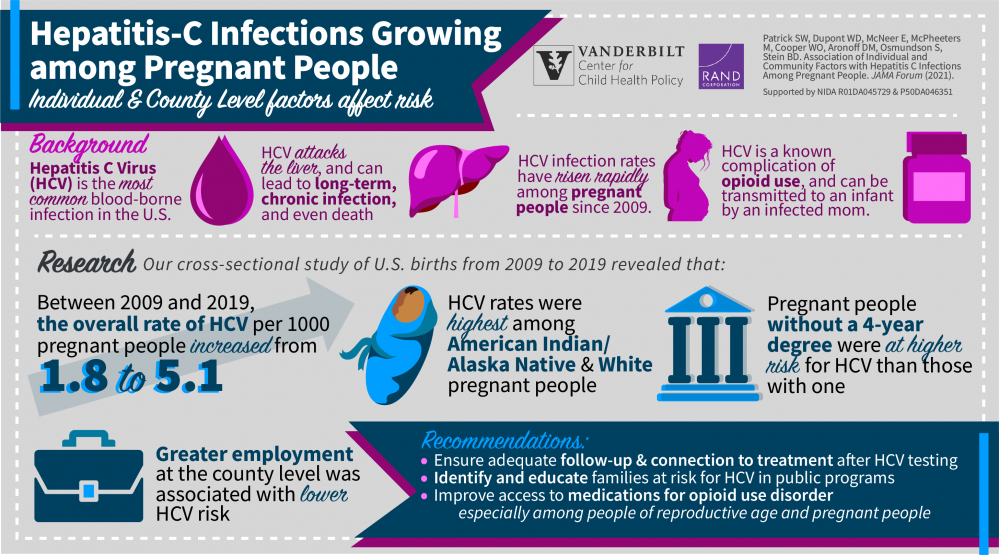
Hepatitis C virus (HCV) infection can lead to long-term health problems including liver damage, liver failure, cirrhosis, liver cancer and even death. These outcomes are especially dangerous for pregnant people and their babies.
The leading cause of HCV in the U.S. is injection drug use as a result of opioid use disorder (OUD), which has seen a rise in most populations, including pregnant people, in recent years. HCV rates have also risen. Between 2009 and 2019, the overall rate per 1,000 live births of HCV in pregnant people increased from 1.8 to 5.1.
To better understand what individual and community factors are associated with HCV infections among pregnant people, researchers at Vanderbilt University Medical Center and the RAND corporation completed a study across all U.S. counties, analyzing a total of 39,380,122 live births.
Scroll down to continue reading...
Continued...
“There hasn’t been a strong focus in recent research on hepatitis C rates in pregnant people,” said Stephen Patrick, MD, MPH, MS, associate professor of Pediatrics and Health Policy and director of the Center for Child Health Policy.
“We don’t often hear about its implications for pregnant people and their infants. We need to talk about it, detect it and implement a tailored approach to treat pregnant people and infants.”
HCV tends to go unnoticed because the disease is “silent.” There are no clinical signs of hepatitis C exposure in infants, but by implementing CDC-recommended universal screenings, clinicians can easily determine who needs treatment.
“Most people can be completely cured of hepatitis C with treatment,” Patrick said. “This is preventable harm.”
The first step to reducing harm for mothers and babies with HCV is getting pregnant people into treatment for OUD, which curbs the risk of HCV. Another way to improve outcomes is to carefully monitor patients after an exposure and connect them to adequate treatment and follow-up. These actions significantly prevent the risk of fatal liver complications later in life for both mothers and babies.
Additional improvements must happen on a community level, said Bradley Stein, MD, PhD, co-author on the paper and director of the RAND-University of Southern California Schaeffer Opioid Policy Tools and Information Center of Research Excellence. The research team’s findings, reported in JAMA Health Forum, show that rural residence, higher rates of employment, and a greater density of obstetricians was associated with a lower risk of developing HCV during pregnancy.
Vanderbilt Study continued...
“Our findings are an important reminder that characteristics of the communities where people live can influence outcomes for pregnant people and babies,” Patrick said. “Particularly for pregnant people at the highest risk, living in communities with more employment opportunities and stronger community connections may mitigate the risk of coming into contact with and developing HCV.”
Researchers noted that pregnant people at highest risk for HCV were American Indian/Alaskan Native and white individuals without a college education. Counties with the highest rates of pregnant mothers and babies with HCV tended to be in the Northeast and Appalachia.
While there tends to be a higher prevalence of OUD and HCV among white pregnant people, health disparities still play a significant role in diagnosing and treating HCV for Black people and their babies.
“Black people are less likely to receive evidence-based treatment for OUD, Black infants are less likely to be tested than white infants for hepatitis C, and Black parents whose infants are placed in foster care for substance exposure are less likely to be reunified with their parents,” said Patrick, who also noted similar disparities likely exist for American Indian/Alaskan Native populations, but this area is understudied.
“As systems are developed to address the rising numbers of mothers and babies affected by HCV, it is critical that interventions are applied equitably to address unequal treatment in these systems of care,” he said.
HCV rates will likely continue to increase as long as rates of OUD also increase, Patrick says. Individual and county-level factors associated with HCV appear to mirror many of the dynamics associated with the opioid crisis.
“Last year, during COVID-19, we had the highest number of overdose deaths we’ve ever had as a nation,” said Patrick. “We still have a long way to go to get control of the opioid crisis as a whole, but as clinicians and policymakers we can take steps to mitigate potential harm now.”
This research is supported by the National Institute on Drug Abuse of the National Institutes of Health under award numbers R01DA045729 and P50DA046351. The content presented in this release is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.